Two health disorders that are commonly misunderstood are osteoarthritis and osteoporosis. While they may sound similar, they are different conditions targeting separate areas of the body with their own distinct symptoms. Let’s compare osteoarthritis vs osteoporosis to see how they impact your health, learn about risk factors and discover which treatments are available.
What is osteoarthritis?
Osteoarthritis (OA) is the most common form of chronic arthritis. It is a painful degenerative joint disease caused by the deterioration of cartilage between bones. In healthy joints, cartilage acts as a shock absorber so bones can glide smoothly. Osteoarthritis breaks down cartilage, causing joint pain and inflammation. It is often referred to as “wear and tear” arthritis. However, it is actually a more complex disorder that affects the entire joint, including the bone, ligaments and tissues.
Osteoarthritis affects more than 32.5 million adults in the U.S. Most sufferers are over age 50, but the disease is prevalent among younger people who have had a prior joint injury. The hands, knees, hips, lower back, spine and neck are the most common areas affected.
Symptoms of osteoarthritis
Symptoms of osteoarthritis develop over time as the cartilage between joints wears away. Someone suffering from osteoarthritis may have one or more of the following issues:
· Painful or achy joints after activity
· Joint stiffness in the morning
· Tenderness in the joints
· Swelling and inflammation around the joint area
· Loss of flexibility
Risk factors for osteoarthritis
Age is the number one risk factor for osteoarthritis. It can also be caused by a joint injury, obesity, weak muscles, genetics or a repetitive stress injury from sports.
Women have a higher risk than men of developing osteoarthritis because of increased weight gain after menopause, hormonal changes and a history of wearing shoes that lack support.
Treating and managing osteoarthritis
There is no cure for osteoarthritis, but it is manageable. People with mild to moderate symptoms can take over-the-counter topical and oral medications to reduce pain. A doctor can prescribe steroids for inflammation.
Exercise is helpful in managing symptoms and reducing body weight, which lessens the burden on joints. Physical therapy can help stabilize joints, increase flexibility and strengthen muscles in the affected areas. A specialist can determine the best course of action, so it is important to see a doctor if you suspect you have osteoarthritis.
What is osteoporosis?
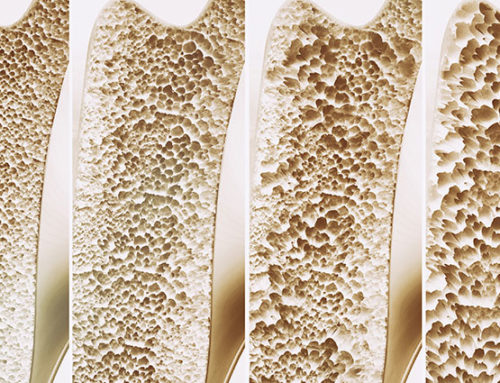
While cartilage deterioration is the key aspect of osteoarthritis, osteoporosis (OP) affects the bone itself. In fact, the word osteoporosis means “porous bone.”
Healthy bones look like a honeycomb underneath a microscope, but osteoporotic bones have larger holes. The decrease in bone mineral density and mass causes them to weaken and be more prone to break.
An estimated 44 million Americans have osteoporosis, and more than half are over 50. Losing bone density is a part of aging, but developing osteoporosis and its symptoms are not. Women are more susceptible than men to osteoporosis due to bone mass loss from hormonal changes.
Symptoms of osteoporosis
Osteoporosis is considered a silent disease because most people do not have symptoms. They may not discover they have the condition until they break a bone. Fractures in older men and women often occur because of osteoporosis. It is common to see these breaks in the hips, vertebrae and wrists after a minor fall.
Advanced osteoporosis can cause a dowager’s hump on the upper spine, or a hunchback, which results from the vertebrae slumping down. Over time, someone with osteoporosis can lose height because the spinal column can shrink.
Risk factors of osteoporosis
There are multiple risk factors for osteoporosis. Gender, family history and specific medical conditions can increase the chances of developing osteoporosis. Lifestyle choices like smoking and heavy drinking can also be factors. Overall, it is more common in:
· Post-menopausal or elderly woman
· Men with low testosterone levels
· People with petite or thin frames
· Anyone with a family history of the condition
· People who take oral steroids regularly
Osteoporosis treatment
Osteoporosis is treatable. A doctor can diagnose the condition after reviewing a person’s lifestyle, health and family history, and by performing blood tests and a bone density scan. Depending on the severity of the condition, drugs can be prescribed to slow bone loss and increase the rate of bone formation.
Taking an active role in treatment by eating a balanced diet rich in calcium and vitamin D is a good start to preventing osteoporosis. Additionally, following an exercise program and giving up unhealthy habits can help maintain bone health and prevent further loss of bone.
Should I see a doctor to find out if I have osteoarthritis vs osteoporosis?
If you are experiencing symptoms of osteoarthritis or osteoporosis, schedule an appointment with a specialist at Cary Orthopaedics right away. We can identify signs of these conditions and create a plan to ease your symptoms and prevent further damage. Our goal is to help our patients get back to a pain-free life.