The emerging field of regenerative medicine is helping patients who have sustained orthopedic injuries or suffer from chronic joint pain. It uses the body’s natural ability to heal itself to treat injuries and diseases of the musculoskeletal system, which includes bones, joints, muscles, ligaments and tendons. In this regenerative orthopedics Q&A, we interview Cary Orthopaedics physician assistant Kevin Morrison, a specialist in the field.
Q: What is regenerative orthopedics?
Morrison: Instead of just treating symptoms or replacing damaged tissues with artificial implants, regenerative medicine aims to stimulate the body’s own repair mechanisms to restore function and promote healing. This can involve techniques such as stem cell therapy and platelet-rich plasma (PRP) injections. Essentially, it’s about harnessing the body’s own healing powers to improve orthopedic health.
Q: What are the types of regenerative orthopedics at Cary Ortho?
Morrison: We offer platelet-rich plasma and stem cell therapy by means of bone marrow aspirate concentrate (BMAC).
Q: How does regenerative medicine work?
Morrison: In orthopedics, regenerative medicine works by using the body’s natural healing processes to repair damaged tissues and promote healing. Here’s a simple breakdown:
- Platelet-rich plasma is a concentration of platelets derived from the patient’s own blood. Platelets contain growth factors and other bioactive molecules that stimulate the healing process at the site of damage.
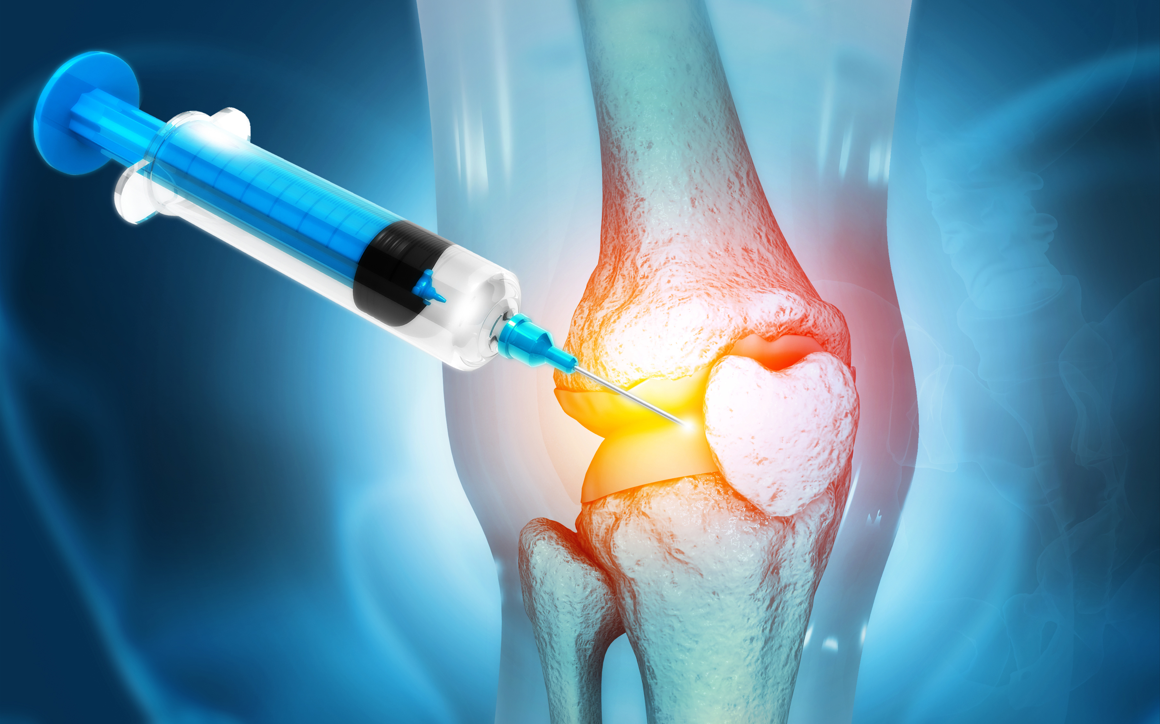
- In PRP therapy, a sample of the patient’s blood is processed to isolate the platelets, which are then injected into the injured area. The growth factors released by the platelets are the mediators that lead to tissue repair.
- Stem cells have the remarkable ability to develop into different types of cells in the body. In regenerative orthopedics, stem cells can be harvested from a patient’s own body (often from bone marrow or connective tissue) and then injected into the site of injury or damage. These stem cells can then differentiate into specialized cells, such as bone, cartilage or muscle cells, to repair the damaged tissue.
Q: Who is a good candidate for regenerative ortho treatments?
Morrison: We treat patients who:
- Have musculoskeletal injuries or conditions that haven’t responded well to traditional treatments like physical therapy, medication or surgery
- Prefer non-surgical or minimally invasive treatment options
- Have relatively good overall health and are not significantly immunocompromised
- Have specific conditions that are known to respond well to regenerative therapies, such as osteoarthritis, tendonitis, ligament injuries or cartilage defects
- Are motivated and committed to following post-treatment rehabilitation protocols to optimize outcomes
It’s essential for patients to consult with their healthcare provider to determine if regenerative orthopedics is suitable for their specific condition, medical history and overall health status.
Q: How do I decide which type of regenerative medicine is right for me?
Morrison: That depends on the injury or condition you have and the goal of the treatment – complete healing versus management of a chronic condition. Your treating provider can help you determine the best option based on the circumstances and the available data surrounding your particular condition or injury.
Q: What conditions does regenerative medicine treat best?
Morrison: We most commonly use stem cell therapy and PRP to treat osteoarthritis given how prevalent it is. It has also shown benefits in acute and chronic soft tissue conditions, like tendonitis.
Q: What is the success rate?
Morrison: Results vary for every type of condition and joint area. Studies are still being conducted with new data coming out and growing more positive every day.
Q: Is there research showing long-term efficacy?
Morrison: We have studies that go back five years specific to arthritis. One study did three PRP injections, one per week over three weeks. The researchers then measured pain scores, functional outcome scores and biomarkers (inflammatory markers) for two years. The patients were evaluated for cartilage progression at five years. The injected group had half as much progression of arthritis compared to the control group (those who did not receive the injection).
Q: Can I still have treatment if I already had surgery on the joint?
Often the goal is to avoid surgical procedures. However, if surgery has already been done and only corrects part of the problem, regenerative orthopedics is a good option. Platelet-rich plasma or stem cells can stimulate better post-surgical healing.
Q: Is the procedure painful?
Morrison: The needle in the knee or other joint may cause immediate but short-lived discomfort. The patient may also experience mild discomfort from the intended inflammatory response of the PRP. That typically resolves within 72 hours.
Q: How many treatments will I need?
Morrison: Most people do a single injection, but there is growing data showing that a series of two or three injections one week apart produces better results.
Q: Are there limitations or risks of regenerative orthopedics?
Morrison: The procedure’s success is not guaranteed. Each individual has a different level of viable platelets or stem cells.
In stem cell therapy, we can’t control how the cells differentiate. For example, in arthritis we want them to become cartilage cells to help fill in any defects, but we can’t artificially direct them toward this specific outcome. We must rely on the people’s internal signaling. In some cases, the body’s environment may be too hostile for the cells to differentiate into the appropriate cells.
Additionally, there is always a risk of infection with any type of injection, but that is very rare. No studies have shown that regenerative therapies could make the problem worse.
Q: How long does it take to work?
Morrison: Most patients see improvement in six to 12 weeks and sometimes as early as three weeks. The greatest effect is typically noted at 12 weeks.
Q: How much does regenerative orthopaedics cost?
Morrison: The costs of regenerative therapies vary depending on the type of injection, number of injections and area injected. For example, PRP for a soft tissue injury often is most effective using a leukocyte-rich PRP injection. This procedure is more complex and, therefore, costs more.
We ask patients to come in for a consultation so we can assess their condition and recommend a course of treatment. At that point, we can provide the costs for PRP or stem cell therapies.
Q: Are regenerative medicine therapies covered by insurance?
Morrison: They are not covered by most commercial insurance because there’s no standardization of these therapies. Since they are relatively cutting-edge, efficacy data is still being collected. However, worker’s compensation and Tricare both cover certain conditions.
Q: Is it FDA-approved?
Morrison: The FDA approved PRP for use in orthopedics in 2009. Stem cell therapy is still considered an investigative procedure. While the FDA monitors it, it has not yet approved it.
Q: Are regenerative medicine treatments safe?
Morrison: As a leading orthopedic practice, Cary Orthopaedics carefully assesses emerging treatment options for safety and efficacy. We responsibly offer viable cutting-edge procedures, like regenerative medicine for orthopedics, to our patients. Based on the increasing number of high-quality clinical trials, PRP and stem cell treatments are deemed to be safe. Study results vary in terms of efficacy, but no data that we are aware of has shown an unsafe profile for patients.
Q: What’s the next step to see if regenerative orthopedics is right for me?
Call Cary Orthopaedics for a regenerative medicine consultation, or fill out an online form to start the appointment process. Get started here.